A continuum of care
‘When it comes to keeping everything in life balanced, our minds are perhaps our greatest asset.’ —Dr Oliver Harrison, CEO, Koa Health
- Authors
- Koa Health
- Publish Date
Mental health encompasses our emotional, psychological and social wellbeing, affecting how we think, feel and the actions we take in our day-to-day lives. It’s important at every stage of life, from birth to adulthood and affects how we handle stress, relate to others and make important choices.
So why don’t we prioritise mental health the same way we do physical health?
Why mental health must be addressed
Among other reasons, mental health must be addressed because mental health and overall health are intrinsically connected: ‘It’s long been known that physical health is a pre-requisite for mental health—mens sana in corpore sano and there’s growing evidence that mental wellbeing also predicts overall health’, says Dr Aleksandar Matic, Director of Research and Development at Koa Health.
And with a worldwide pandemic affecting how people work, play, live and even how they seek out care, we can’t just sweep mental health under the rug any longer. The need for a continuum of care that covers a wide range of mental health issues has never been more pressing.
- In the Dunedin Study, which followed over a thousand participants in New Zealand from birth until middle age, 83% of participants experienced mental health issues ranging from temporary periods of overwhelming stress to more serious, chronic conditions by middle age.
- Per Mind UK, in 1 in 4 people experience a common mental health problem every year.
- The World Health Organization (WHO) estimates someone dies by suicide every 40 seconds worldwide.
- As of July 2020, 53% of Americans reported their mental health had been negatively impacted by stress and worries related to Covid-19, up from 32% in March (The Kaiser Foundation).
Furthermore, stress and poor mental health are linked to additional problems with overall health: ‘Mental health conditions can make symptoms of physical health conditions such as diabetes, heart disease and others worse, and vice versa’, says Content Lead at Foundations, Dr Sophie Dix. Covid-19 has only made this situation worse—per the CDC, stress during an infectious disease outbreak can cause the following:
- Fear and worry about your health and the health of loved ones
- Worries about your financial situation and your job
- Disrupted sleep and eating patterns
- Difficulty sleeping and concentrating
- Worsened chronic health problems/mental health conditions
- Increased tobacco, alcohol and other substance use

The gap in existing care
57% of people with a mental illness go untreated in a given year. Why? Potentially as a result of barriers to care: Financial constraints, limited time and difficulties with access (such as having to drive over an hour to get to a specialist) are major contenders, along with the stigma and embarrassment often associated with mental health conditions.
Unfortunately, beyond these barriers, there are also known shortages and problem points in the existing care systems affecting people’s ability to access appropriate support. As of 2021, the Royal College of Psychiatrists perceived the following effects of existing shortages:
- Only 1 consultant psychiatrist per 12,567 people
- 1.5 million waiting for mental health treatment in England
- £1.73 billion needed to fund the extra medical school places needed to fill the demand for qualified professionals by 2029
These issues will only create wider gaps in care for everyone and make it that much harder for people to access the right treatment at the right time. And when people go without the mental health support they need, it’s hard for them to go about their lives and even harder for them to thrive.
How can gaps in care be covered?
Busy clinicians and medical professionals work hard to help as many patients as possible. Still, the majority are at (and even beyond) capacity when it comes to face-to-face therapy and treatment options. Can digital therapeutics extend their reach and help them care for more patients?
In a word, perhaps. As psychiatric services in general make the shift from hospitals and specialised centres to community and technology continues to progress, support delivered via device is becoming a viable alternative to in-person care.
Not only have techniques validated in clinical practices (such as cognitive behavioural therapy or CBT) been shown to be effective when delivered via app, studies also show that people (of all ages) are open to technology-based interventions:
- More than 75% of people are willing to use digital health care services (McKinsey & Company)
- 7 out of 10 people of all ages are open to technology-enabled care (Deloitte)
- 81% of people in the US and 79% of people in the UK own a smartphone (and can potentially access app-based care)
Support delivered via personal devices makes sense: ‘Digital therapeutics can allow clinicians to provide quality care with fewer face-to-face sessions and in some cases no face-to-face care at all, allowing them to help more people while reducing cost’, says Stephen Dunne, CDTxO (Chief Digital Therapeutics Officer), at Koa Health. In addition to being easier to access and typically more economical than in-person care, this type of support also encourages people to become more proactive about their mental health with mental wellbeing tools they can use when (and where) they need them.
What is Koa Health doing to close these gaps?
Our team is putting our years of experience in behavioural and data sciences, mental health and product development towards the creation and iteration of practical, evidence-based digital therapeutics and wellbeing tools. Our mission? To help employers, healthcare providers and insurers support mental health for employees, patients and members.
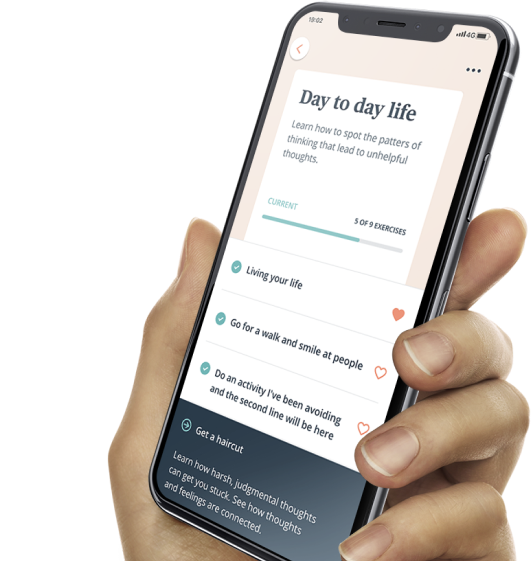
How do we plan to achieve this goal? Our approach focuses on a sliding scale of support, from solutions for general mental wellbeing support (such as Foundations) to tools to help clinicians treat patients with moderate to severe mental conditions (for example, Perspectives). Designed to be practical, accessible and easy-to-use, our evidence-based solutions address a spectrum of mental health issues, as well as all-too-common pain points for patients, providers, and insurers.
What challenges are you facing when it comes to providing a continuum of care? Let us know at info@koahealth.com.
about the author

Koa Health
The Team @ Koa Health
Our diverse team of developers, researchers, psychologists and behavioral health experts work together to create practical, thought-provoking content to accompany our range of digital therapeutics.
